- Cracking the (Reimbursement) Code: New @AGSJournal Editorial Outlines Decade of @AmerGeriatrics Hard Work, Big Changes to Advance Covering #Geriatrics Care We Need as We Age http://ow.ly/6XQM30m6hnn
New York (Oct. 4, 2018)—For millions of older adults who rely on Medicare, the federal health insurance program for people 65-years-old and older, it happens seamlessly and almost always behind-the-scenes: The care we receive from expert clinicians becomes five-digit “billing codes,” which in turn ensure our clinicians can be reimbursed for their work supporting our health, safety, and independence. But even billing codes have a story to tell—an important one at that, as experts from the American Geriatrics Society (AGS) describe in a new Journal of the American Geriatrics Society (JAGS) editorial (DOI: 10.1111/jgs.15593). The editorial outlines how several key health services—from those for managing chronic care to those for assessing cognitive health—came to be recognized as part of Medicare through an important but oft unsung facet of geriatrics expertise: its leaders’ engagement in building a better public policy environment to support the care we all need as we age.
“It’s hard to believe but as recently as the late 1990s, Medicare—our primary federal insurer for older people—lacked the means to reimburse or even recognize several core services essential to older Americans,” notes Peter Hollmann, MD, AGSF, AGS Treasurer and one of the lead authors for the retrospective editorial. “In reviewing which forces and what players were instrumental to AGS-led change from then to now, we hope geriatrics health professionals and older adults alike will have a better appreciation for what it takes to improve care by making sure it can be recognized—particularly at a time when more of us than ever before will need access to new, innovative health services.”
As the editorial authors explain, much of that work began with an investment by the AGS of time, talent, and resources in two important entities: the Current Procedural Terminology (CPT) Editorial Panel and the Relative Value Scale Update Committee (RUC), both coordinated by the American Medical Association (AMA).
Though you may not know the CPT Editorial Panel or RUC by name, you are certainly familiar with their work. Respectively, they develop and continually review billing codes (referred to as “CPT codes”) for health services and procedures and ensure reimbursement for those codes accurately reflect provider work. Together, these groups shape what services Medicare will cover (and at what value) from one year to the next.
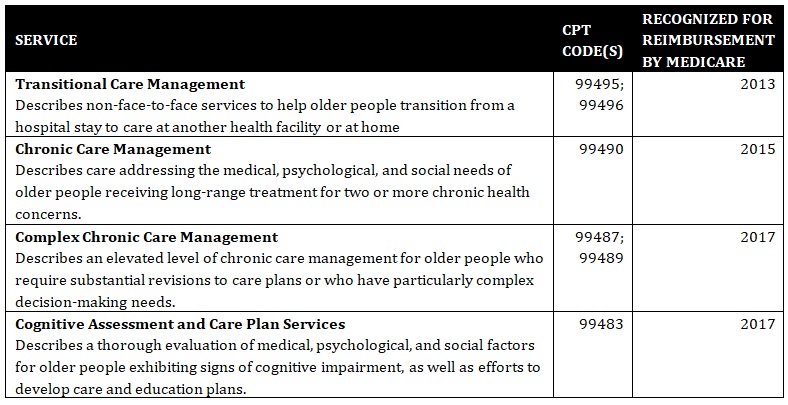
The AGS editorial presents a case study in working with groups like the CPT Editorial Panel and the RUC to ensure our clinicians are able to implement best practices to health care because these services can be tracked and reimbursed appropriately. Around 2011, the AGS became actively involved in the work of the CPT Editorial Panel and RUC. Since then and with significant support from the AMA and several key medical societies, the AGS had been instrumental in securing recognition and reimbursement for several of today’s most important geriatrics services. These include:
“In working to develop, review, and ensure approval for these codes and other components of our public policy work, we’ve learned a great deal—particularly about the importance of a clear vision to improve health, safety, and independence for older people,” Dr. Hollmann observed. “We set out in the 1990s to achieve appropriate payment for the care of older people. We are proud of our successes to-date, but we also recognize the need to better describe and value the work for geriatrics health professionals moving forward.”
As for what lies immediately ahead: CMS’s proposed Medicare Physician Fee Schedule for 2019 (released in July 2018 and outlining changes to payment policies for the next calendar year) included some sweeping—and potentially disconcerting—changes to the evaluation and management codes, which encompass many of the core services health professionals provide in routine office visits. AGS experts submitted comments to CMS and Congressional leaders on the proposed rule, and also outlined the extensive process for preparing insights and recommendations in a separate article also published in the JAGS (DOI: 10.1111/jgs.15651).
“While the new system streamlines the billing process,” AGS President Laurie G. Jacobs, MD, AGSF, explains, “it does so by reducing payment for the care of particularly complex patients like older adults, who have traditionally been categorized at higher levels because of the work that goes into addressing their complex needs. Reducing the burden of documentation is important, but adequate payment for complex care—reflected in the types of codes we’ve developed in the past—is absolutely essential.”
Both AGS editorials, “Hard Work, Big Changes: AGS Efforts to Improve Payment for Geriatrics Care” and “Putting Complex Older Persons First: How the CMS 2019 Payment Proposal Fails Older Americans,” are available for free from JAGS. For even more information on AGS efforts to improve Medicare, Medicaid, and payment and services for older people, visit AmericanGeriatrics.org/Where-We-Stand.
AGS ACTION POINTS
- As late as the 1990s, Medicare—our primary federal insurer for older people—lacked the means to reimburse or even recognize several core services essential to older Americans.
- Today, services as diverse as Transitional Care Management (for helping bridge older adults from a hospital stay to care elsewhere) to comprehensive assessment and care planning for those living with cognitive impairments are a reality thanks to the important but oft unsung work of geriatrics experts committed to a Medicare payment system that supports us all as we age.
- For that work to continue moving forward, policymakers, fellow health professionals, and older adults alike must continue to focus on improving existing payment systems to support care for all Americans, including the seriously ill.
About the American Geriatrics Society
Founded in 1942, the American Geriatrics Society (AGS) is a nationwide, not-for-profit society of geriatrics healthcare professionals that has—for more than 75 years—worked to improve the health, independence, and quality of life of older people. Its nearly 6,000 members include geriatricians, geriatric nurses, social workers, family practitioners, physician assistants, pharmacists, and internists. The Society provides leadership to healthcare professionals, policymakers, and the public by implementing and advocating for programs in patient care, research, professional and public education, and public policy. For more information, visit AmericanGeriatrics.org.
